Squamous cell carcinoma is the second most common skin cancer. Think of it as the middle child of skin cancers — it’s not the same as basal cell carcinoma (the most common), and it’s not as unpredictable as melanoma (the third most common). In fact, a lot of people gloss over it altogether.
But squamous cell carcinoma is nothing to ignore. In fact, the more you know about it, the better your chances of preventing and treating it.
Like basal cell carcinoma, squamous cell carcinoma is a type of epithelial carcinoma, meaning it forms on the outer tissue of the skin. It’s most commonly found in the mouth and in the other mucous membranes. It appears less frequently than basal cell carcinoma (about two in ten skin cancers are considered squamous cell carcinoma), but it’s potentially more aggressive than basal cell carcinoma. As it gets larger, it gets more complex and tends to be more painful.
The bigger it gets, the faster it grows. Once it grows to over two centimeters in diameter, it has a much higher rate of metastasis. Like any form of cancer, the earlier we can detect it, the easier we can stop it from spreading.
How Do I Know If I Have Squamous Cell Carcinoma?
Squamous cell carcinoma typically begins in one of three ways:
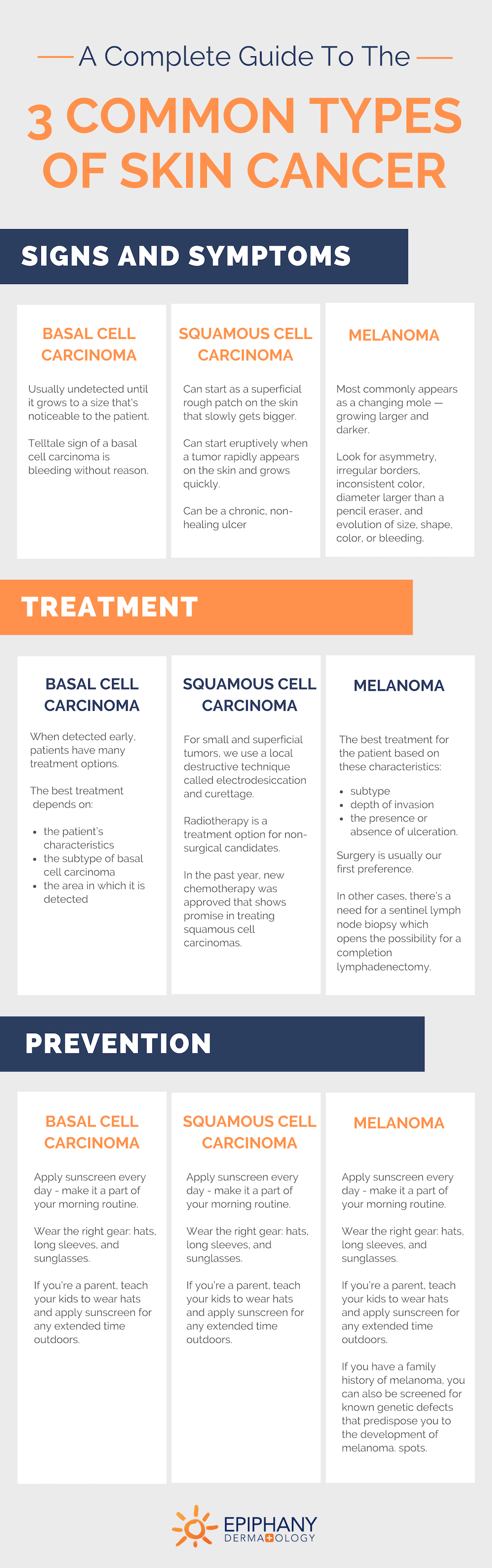
- It can start as a superficial rough patch on the skin that slowly gets bigger.
- It can start in an eruptive way, when a tumor rapidly appears on the skin and grows quickly.
- It can be a chronic, non-healing ulcer the patient either neglects or is unable to remedy with at-home care.
If you have any of these types of places on the skin, see a dermatologist stat so they can begin treatment right away.
Risk Factors for Squamous Cell Carcinoma
Like most skin cancers, chronic sun exposure drastically increases your risk of developing squamous cell carcinoma, especially if you have fair skin.
But the sun isn’t the only cause of squamous cell carcinoma. Squamous cell carcinoma is clearly driven by the human papillomavirus (HPV).
When it appears in the head and neck area, especially in the mucous membranes, it’s been driven by smoking and drinking — particularly in combination.
Transplants and other cancers also increase the risk of getting this disease. Squamous cell carcinoma becomes the predominant type of skin cancer over basal cell carcinoma in transplant patients when they undergo immunosuppression to protect their transplant. Also, immunosuppressed patients with leukemia or lymphoma are predisposed to squamous (and basal) cell carcinoma. Patients with these conditions should be on high alert for any suspicious lesions on the skin and should regularly visit their dermatologist.
Squamous Cell Carcinoma Treatment
Fortunately, there are multiple squamous cell carcinoma treatment options with the potential to completely cure this cancer. As a rule, squamous cell carcinoma is first considered a surgical problem. For small and superficial tumors, we use a local destructive technique called electrodesiccation and curettage (also referred to as EDC, ED & C, or C & E).
For very small, superficial lesions we consider topical chemotherapy but usually opt for a Mohs surgery excision instead. In this technique, we apply local anesthesia, then scrape the base of the tumor. We take a 4-mm margin around the diagnosed squamous cell area and process it with frozen horizontal sections. In about 15 minutes, we can determine if the surrounding margins are positive or negative. If any positive margins remain, we can repeat the process to clear the carcinoma.
Radiotherapy is a squamous cell carcinoma treatment option for non-surgical candidates. With regular radiotherapy treatments over the course of three to six weeks, we can target these radio-sensitive areas and eliminate most of the cancer cells.
In the past year, new chemotherapy was approved that shows promise in treating squamous cell carcinomas that are either locally aggressive or metastatic with some degree of efficacy. If other treatments aren’t an option for you, your dermatologist may recommend this new treatment.
Squamous Cell Carcinoma Prevention
Skin cancer prevention always starts with sun protection. No, you can’t undo the damage that’s been done to your skin cells. But it’s never too late to start applying sunscreen and wearing protective gear for your time in the sun.
Apply sunscreen every day. Make sunscreen application part of your morning routine. Then you’re protecting yourself from the rays throughout the day, even if the only sun exposure you plan to get is through a window.
If you’re a parent, start instilling good sun protection practices for your kids at an early age. Make sun protection a habit in your home. Just like you teach your kids to grab a jacket if it’s cold, teach them to grab a hat and apply their sunscreen when they’re in the sun. Yes, we want our kids to be outdoors, but we want them to be safe while they’re out.
Unfortunately, squamous cell carcinoma prevention isn’t completely in our control. There are other health factors (like leukemia, HPV, and organ transplants) that play a role in the spread of this disease. However, with early detection, sun protection, and a skin care specialist to walk you through treatment, we have a high chance of curing it.

Dr. Adrian Guevara is a board-certified dermatologist in El Paso, TX. As a Fellow of the American Academy of Dermatology and the American Society for Mohs Surgery, Dr. Guevara has served the extended El Paso and Las Cruces region since 2006. In his spare time, Dr. Guevara enjoys spending time with his family and playing tennis.

